Interferential

Combination
Back Overview and description of the therapeutic applications
1. Sub-acute per arthritis humero-scapularisI Interferential (2-pole; AMF 100 HZ; spectrum 100 hz spectrum time 6 s; contour 50%
Treatment time :15 minutesSuggested advice : intensity pleasantly noticeable
Treatment frequency : 5x per week.
2 Chronic lumbago
Interferential (2-pole); AMF 10 Hz; spectrum 90 hz spectrum time 6 s; Contour 100%
Treatment time : 10 minutes
Suggested advice : intensity strongly noticeable.
Treatment frequency ; 3x per week
3 Arthrosis
Interferential (2- pole); AMF 50 Hz, spectrum 50 Hz spectrum time 6s; contour 1 %)
Treatment time; 12 minutes
suggested advice; intensity well noticeable.
Treatment frequency; 3x per week.
4 Contractures after immobilization
Interferential (2- pole); AMF 2 Hz, spectrum 10 Hz spectrum time 6s; contour 100 %)
Treatment time; 15 minutes
suggested advice; intensity to be increased until rhythmic contraction occur
Treatment frequency; daily
5 Post-operative pain
Tens continuous (Pulse duration 50 ms; pulse frequency 100 hz; spectrum 50 hz; spectrum time 6 s; contour 50%
Treatment time ; 15 minutes.
suggested advice : intensity just noticeable.
Treatment frequency; daily
6 Neuralgia
Tens continuous (Pulse duration 50 ms; pulse frequency 75 hz; spectrum 50 hz; spectrum time 6 s; contour 50%
Treatment time ; 20 minutes.
Suggested advice : intensity just noticeable.
Treatment frequency; daily
7 Herpes zoster
Tens continuous (Pulse duration 50 ms; pulse frequency 75 hz; spectrum 50 hz; spectrum time 6 s; contour 50%
Treatment time ; 10 minutes.
suggested advice : intensity just noticeable.
Treatment frequency; daily
8 Epicondylitis humeri lateralis- manifesting radiation in extensors
Tens continuous (Pulse duration 200 ms; pulse frequency 80 hz;spectrum 50 hz; spectrum time 6 s; contour 100%
Treatment time ; 10 minutes.
suggested advice : intensity just noticeable.
Treatment frequency; daily
9 Actual segmental disarticulations
Tens continuous (Pulse duration 80 ms; pulse frequency 50 hz; spectrum 100 hz; spectrum time 6 s; contour 100%
Treatment time ; 25 minutes.
suggested advice : intensity just noticeable/ pleasant tingling sensation
Treatment frequency; 5 x per week
10 Tension headache
Tens continuous (Pulse duration 100 ms; pulse frequency 100 hz; burst frequency 2 hz)
Treatment time ; 15 minutes
suggested advice : intensity well noticeable.
Treatment frequency; 3 x per week
11 Circulation-disorders - calf- muscles
Tens continuous (Pulse duration 200 ms; pulse frequency 100 hz; burst frequency 2 hz)
Treatment time ; 15 minutes.
suggested advice : intensity well noticeable.
Treatment frequency; 3 x per week
12 Acute muscle rupture
Ultrasound therapy (treatment head 4 cm2; 1 MHZ; duty-cycle 1:4;intensity 0.8 w/cm2
Treatment time : 7 minutes .
Suggested advice: intensity just noticeable
Treatment frequency; 3x per week.
13 Epicondylitis laterals - low actually
Ultrasound therapy ( treatment head 4 cm2; 1 MHZ; duty-cycle 1:1;intensity 0.4 W/cm2)
Treatment time : 7 minutes.
suggested advice: intensity just noticeable.
treatment frequency :3x per week.
14 Injury medical collateral ligament art. Genus
Ultrasound therapy (treatment head 4 cm2; 1 MHz; duty-cycle 1:4 ;intensity 1.5 W/cm2)
intensity time :20 minutes.
suggested advice : intensity just noticeable.
Treatment frequency : 3x per week
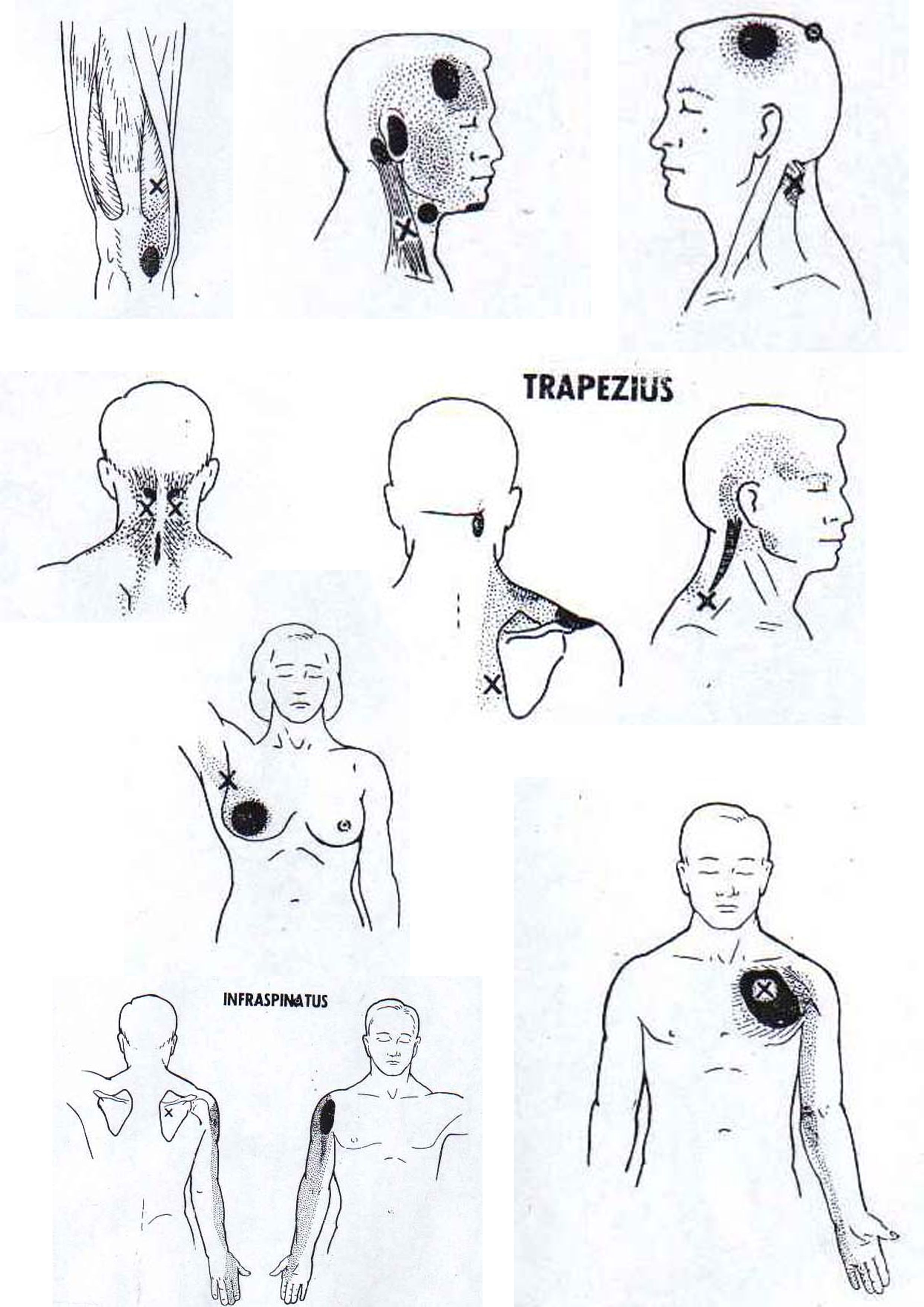
15 Detection of pain-points
Combination therapy: interferential (AMF 100 Hz; spectrum 0hz)and Ultrasound therapy (treatment head 4 cm2 , 1 MHZ;duty-cycle 1;1 intensity 1.0 W/cm2)
Treatment time : 20minutes
Treatment advice: intensity well noticeable. The treatment time depends on the size of the body area to be treated.
16 chronic lumbago
Interferential (2-pole); AMF 10 Hz; spectrum 90 hz spectrum time 6 s; Contour 100%
Treatment time : 10 minutes
Suggested advice : intensity strongly noticeable.
Treatment frequency ; 3x per week
17 Gonarthrosis
Combination therapy: interferential (AMF 100 Hz; spectrum 50 hz; spectrum time 6 s; contour 1%) and ultrasound therapy (treatment head 4 cm2 1 MHZ; duty-cycle 1;4; intensity 0.5 W/cm2)
Treatment time : 7 minutes.
suggested advice : intensity well noticeable.
Treatment frequency: 3x per week
18 Chronic distortion pedis
combination therapy: tens continuous (pulse duration 50 ms; pulse frequency 100 hz; contour 1%) and ultrasound therapy (treatment head 4cm2, ! MHz; duty-cycle 1:4; intensity 0.5 W/cm2
Treatment time :7 minutes.
Suggested advice: Intensity well noticeable.
Treatment frequency: 3x per week
19 Ischialgy
combination therapy; tens continuous (pulse duration 50 ms; pulse frequency 100 hz; contour100%) and ultrasound therapy (treatment head 4 cm2 1 MHz; duty-cycle 1:1; intensity 0.5 W/cm2)
Treatment time : 10 minutes
suggested advice: Intensity noticeable
treatment Frequency; daily
20 Acute subluxation humeri
Combination therapy; tens continuous (pulse duration 50 ms; pulse frequency 100 hz; contour100%) and ultrasound therapy (treatment head 4 cm2 1 MHz; duty-cycle 1:1;intensity 1.0 W/cm2)
Treatment time : 5 minutes
suggested advice: Intensity just noticeable
treatment Frequency; daily
Ultrasonic

Triggerpoint
Physiotherapy staffing
Staffing of Physiotherapy Department
PHYSIOTHERAPY MANAGER OR DIRECTOR.is
SENIOR PHYSIOTHERAPIST (To supervise basic P. T & reports to Manager). PHYSIOTHERAPIST (To supervise physiotherapy assistant maintenance of record). PHYSIOTHERAPY ASSISTANT.(To supervise helper& Pt. Communication feedback to Physiotherapist).
HELPERS (Pt. Communication feed back to Physiotherapist).
UP GRADATION OF PHYSIOTHERAPY
Once pt. Is being admitted in the hospital it means his physical condition deteriorated day by day. So every pat. Before discharge from the hospital must have physiotherapy advice including home exercise prong. Once pat. Is being referred in Physiotherapy department he must be evaluated documented properly purely in professional manner than treated, progress, follow up and record must be maintained.
Physiotherapy does not mean simply exercises and operation of machine that can be done by Physiotherapy assistant, they are especially trained in various exercises and operation of machines, they must work under supervision of qualified Physiotherapist trained in various specialty.
Qualified Physiotherapist means to advice, explain patient problem, disability to discuss physical complication related to patients medical hindrance, to evaluate patient physical disability to monitor progress.
INVOLVEMENT OF PHYSIOTHERAPIST
Evaluate patient professionally.
Plan & implement physiotherapy treatment.
Provide home exercise program.
Monitor progress of pat.
Supervise & educate Physiotherapy Assistant.
PHYSIOTHERAPY INVOLVEMENT WITH HOSPITAL STAFF
To arrange courses for Nursing staff.
Lifting & transfer pat. Which makes nursing staff affective with minimal Physical strain to their body.
To organize various ergonomically meetings with various staff to make hospital staff members less Physically strained.
Monitor progress of pat.
Supervise & educate Physiotherapy Assistant.
DUTIES OF SENIOR PHYSIOTHERAPIST
To arrange meetings with patients family if needed to educate physical disability, documents and maintain record meetings.
Provide guidelines to basic Physiotherapist in their respective fields. Rotate physiotherapist monthly in various field.
Provide unto update knowledge about know how in the world of physiotherapy by the help of Internet.
Maintain discipline in the dept.
Maintain standard & behavior with staff and patient.
Solve various complains related to staff, Patient and physiotherapy Assistant.
To monitor and supervise relations of patients those who are not satisfied with the treatment.
DUTIES OF PHYSIOTHERAPY DIRECTOR/MANAGER
Look after welfare of organization.
Submit reports of Physiotherapy department monthly.
Maintain relation with various consultants.
Answerable to various consultants.
Look after hazards in departments & discuss with legal advisor .Upgrade standard.
Concentrate marketing of Physiotherapy departments.
To improve economy of department.
Discuss departmental problems with Senior Physiotherapist.
Supervise planning of Physiotherapy departments.
To upgrade unto International standard & concentrate on International market.
TO UPGRADE PHYSIOTHERAPY IN THE FIELD OF
Psychiatry
Gynecological conditions
Geriatric conditions
Burns
Urology
Wheel chair and ADL standard
Ergonomically evaluation of various companies senior executives to decrease physical strain.
Shoulder
Flexion
1.Pectoralis major (med. & pect. Nerve C5-T1)
2.Anterior deltoid (Maxillary Nerve C5-C6)
3.Supraspinatus (Suprascapular nerve C5)
4.Biceps brachii (musculocutaneus nerve C5-C6)
5.Coracobrachialis (Musculocutaneus nerve C6-C7)
6.Subscapularis (upper & lower sub scapular nerve C5-C6)
Extension
1.Latissimus dorsi (thoracodorsal nerve C6-C8)
2.Triceps brachii long head (Radial nerve C7-C8)
3.Posterior deltoid (auxiliary nerve C5-C6)
4.Teres major (lower sub scapular nerve C5-C6)
5.Subscapularis (upper & lower sub scapular nerve C5-C6)
Abduction
1.Middle deltoid (auxiliary nerve C5-C6)
2.Supraspinatus (Suprascapular nerve C5)
3.Infraspinatus upper fibre (Suprascapular nerve C5-C6)
Adduction
1.Latissimus dorsi (thoracodorsal nerve C6-C8)
2 Pectoral is major (med. & pect. Nerve C5-T1)
3.Teres major (lower sub scapular nerve C5-C6)
4.Triceps brachii long head (Radial nerve C7-C8)
5.Teres minor(axillary nerve C5)
6-Infraspinatus lower fibre (Suprascapular nerve C5-C6)
Int.Rotation
1.Latissimus dorsi (thoracodorsal nerve C6-C8)
2.Pectoralis major (med. & pect. Nerve C5-T1)
3. Subscapularis (upper & lower sub scapular nerve C5-C6)
4. Teres major (lower sub scapular nerve C5-C6)
5. Deltoid ventralo fibers (Auxiliary Nerve C5-C6)
Ext. Rotation
1. Deltoid dorsal fibers (Auxiliary Nerve C5-C6)
2. Infraspinatus (Suprascapular nerve C5-C6)
3. Supraspinatus (Suprascapular nerve C5)
4. Teres minor (auxiliary nerve C5)
